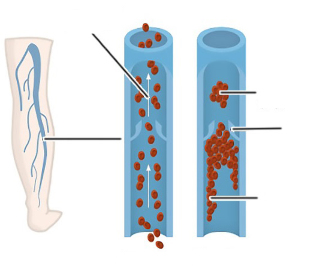
Varicose veins is a disease characterized by changes in the state of veins in the legs and impaired blood flow. When the form is ignored, blood vessels can bulge, which can cause swelling and soreness of the limbs (under load) and aesthetic discomfort. At this stage, surgical removal of the damaged vein is effective.
Indications of varicose vein surgery
Varicose vein surgery can only be performed when there are signs of removal of blood vessels:
- Varicose veins affect most veins;
- Severe soreness and swelling of the legs during physical exercise interfered with normal lifestyle;
- The formation of open wounds and ulcers in the context of disease development. Secondary infections are dangerous.
- Violation of the permeability of blood through blood vessels, often accompanied by convulsions;
- Significant development of vascular necrosis;
- Pathological changes in veins, accompanied by their expansion and protrusion. This change can be dangerous due to vascular injury, and it can also cause aesthetic discomfort;
- Blood clots in the veins.
Surgical intervention is only allowed in the case of advanced forms of varicose veins and conservative treatments without dynamics.
Absolute and relative contraindications of surgical contraindications
Not only in the case of indications, but also in the case of no contraindications, surgery to remove varicose veins in the legs. When holding a child, it may also violate the condition of the leg veins. After childbirth, the pathology usually disappears by itself. In the case of contraindications, surgical intervention can increase the patient's condition and even fatal consequences, so it is dangerous. Venectomy is a surgical procedure to remove damaged veins and restore normal blood flow in deep veins. The circulatory system of the legs is composed of deep veins and many branches of superficial veins, which can affect varicose veins. Due to valve dysfunction, blood vessel activity changes. During the normal operation of the blood vessel, the valve is closed to ensure that blood flows in only one direction. In those veins affected by varicose veins, the valves will not close. As a result, the blood can move in both directions, resulting in impaired blood flow, blood congestion and vein protrusion. In order to restore the blood supply to the limbs, it is necessary to eliminate the affected vein (reverse blood flow), that is, perform a phlebectomy. Before the operation, the patient should be prepared (check up, scan the vein status, determine the patient's overall condition). If there are no contraindications, the specialist will perform surgery, including the following stages: The operation is performed under general or local anesthesia. It depends on the size of the vessel and its location. Surgical removal of veins was used in different stages of varicose vein formation. The procedure is very effective (over 98%). The restoration of blood circulation occurs in a short time. The effectiveness of surgery depends not only on the qualifications of the surgeon, but also on the compliance with the rules of surgery during the postoperative period. After phlebectomy, you need: If you follow the rules, you can fully recover limb function within 6 months. When direct blood vessels with a diameter of at least 0. 02 cm are affected and the number of capillaries is small, a laser will be performed to remove varicose veins in the legs. The procedure involves applying light waves to the damaged container, followed by welding and destruction. Any of the following three types of optical fibers can be used for vein laser coagulation: The choice of equipment should not only be decided by the patient, but also by the attending physician based on the vascular status. Before selecting EVLK by a phlebologist (an expert who examines veins and eliminates varicose veins), the characteristics of the damaged blood vessel must be determined. They must be straight and at least 2 mm in diameter. As a result, laser therapy can be applied to the following groups of blood vessels: Other veins can only be treated by venectomy. Using 3 types of fibers, veins can be removed by the EVLK method. Depending on the type of equipment, the treatment effect will vary. When the end light guide plate is used for surgery, the effectiveness of the treatment is 94-96%. The operation using radial light guides can achieve 100% elimination of varicose veins in the legs. When choosing to use EVLK to remove varicose veins, patients should undergo the following training: Before starting the operation, please mark the boundary of the damaged blood vessel, the location where the laser/fiber is inserted, and the location of the branched capillary. These marks allow you to weld the beginning and end of veins and the exit of capillaries. This process is carried out under the control of an ultrasonic machine. EVLK is produced in stages: After completing this process, the patient can leave the hospital immediately. In order to restore the function of the injured limb and prevent the development of complications, you need to be familiar with the nuances of rehabilitation after EVLK. They are: If varicose veins still need to be removed, surgery is allowed within 7 days. Depending on the type of intervention, surgery to remove leg varicose veins has the following advantages: Since the incision/puncture is small, the risk of infection during the operation is minimal. There is a risk of complications after vein removal by surgery or laser. Adverse reactions may be due to low qualifications of experts or violations of regulations during the recovery period. Possible complications of venectomy and venous coagulation. During both operations, allergic reactions to anesthetics may occur. Surgery to remove leg veins with varicose veins is sometimes accompanied by complications. To prevent them from occurring, you need to do the following: If unacceptable deviations are found during this operation, you must contact the clinic immediately. The two methods of removing leg veins are more than 95% likely to recover completely, but to eliminate contraindications, follow the rules during the recovery period and when choosing a validated clinic. Through surgical treatment, the blood flow and external conditions of the legs were restored after three months, and through laser treatment, it returned to normal after 30 days. In the advanced form, the removal of blood vessels is performed surgically. The treatment method depends not only on the patient's wishes, but also on the indications and contraindications of the operation. The effectiveness of treatment depends on the qualifications of the doctor and the implementation of postoperative foot care rules.absolutely prohibited operation
List of relative prohibitions
Stable blood pressure
The existence of infectious diseases
Blood pressure often rises
Skin pathology affecting the skin of the legs
Chronic heart disease
The inflammatory process in the body including blood vessels
Seniors after 70
Recovery period after other surgical operations
The existence of cancer
Chemotherapy
Diabetes and severe asthma
Severe soft tissue damage caused by trauma
Thinning and fragile blood vessels
Acute liver and kidney disease
Patients with limited leg movement (paralysis) or bedridden
Coagulation disorder or anemia
The final stage of varicose veins
Taking hormones, antibiotics or other stimulating drugs
There is a complicated leg fracture (damaged blood vessels and nerve endings)
Overweight
Allergic reaction to drugs used in surgery
The patient refused the operation
Vein extraction
Anatomical significance, the technique of major surgery to remove veins
Efficiency level
Rehabilitation

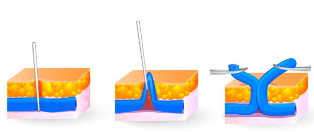
Use laser for vein coagulation
Equipment

Fiber type
Introduction to operation
Ending (Classic)
This kind of fiber produces beam radiation from the end, that is, the container is sealed on the front. The disadvantage is the formation of hematoma and the pain of tight veins. The maximum vein diameter is 0. 1 cm.
Radial (Elf painless radial light guide)
The light waves from the optical fiber form a circle with a diameter around the vein. This allows for the treatment of veins of any size. Moreover, the risk of hematoma formation and edema is minimized.
Three types of radial fiber
A laser with two halos is used to eliminate varicose veins. The first one prepares the vein for surgery (eliminates excess fluid), and the second circle welds the wall. For treatment, light guides for fine and short veins and large blood vessels were made.
Which veins can be removed using the EVLK method
Efficiency
Preparation and implementation phase

Rehabilitation function
Advantages of each method

Vein extraction
EVLK
The surgical incision is about 5 mm, so there is almost no scar
No pain during the operation (using local anesthesia). No need for general anesthesia
The painless operation is performed under local anesthesia. For small fibrillectomy, local anesthesia is used.
EVLK is executed under ultrasound control. The result is high precision and high efficiency.
Low cost
There is little or slight hematoma and pain at the surgical site.
Fast recovery of skin tone (purple violet shade without stars and epidermis)
This operation requires 1 puncture, so no sutures and scars are needed
Short recovery time of about 30 days
The longest recovery period is 5 days
Effective for all forms of varicose veins
After the operation, the patient can leave the clinic within 1 hour.
can return to normal life within 24 hours.
EVLK can be performed when the ulcer damages the integrity of the epidermis.
The duration of surgery does not exceed 40 minutes.
EVLK can complete leg training in one day. One foot was allowed a second operation after 7 days.
Complications after surgery and laser vein surgery

Vein removal method
Minor complications caused by the procedure
Major complications
Vein extraction
Vein laser coagulation
Measures to reduce complications

Forecast comparison























